Pancreas Transplant: Indications And Risks
Organ transplantation is a medical procedure that aims to replace a damaged organ with a healthy one. In 2016, 53,345 were performed across America, according to the Pan American Health Organization. I the pancreas keeps track of the highest success rates.
The pancreas is an abdominal organ that participates in the production of digestive enzymes and hormones to control blood sugar levels. Pancreas transplantation greatly improves the prognosis and quality of life of patients with severe diabetes mellitus, reducing the complications of the disease.
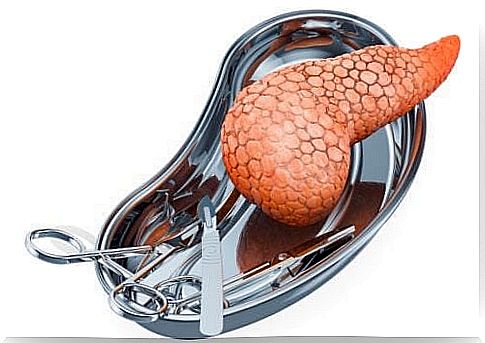
What is a pancreas transplant?
Pancreas transplantation is a surgery in which a healthy and functional pancreas is implanted, replacing a damaged or inefficient one. This surgery can be performed in isolation, although it has been shown that in 88% of cases it is performed simultaneously with a kidney transplant.
The pancreas is taken from a donor diagnosed with brain death; once extracted, it can be transported in a container with a cooling system for a maximum period of 20 hours.
Pancreatic transplant surgery takes about three hours. The donated organ is placed in the lower right part of the abdomen. The diseased pancreas, on the other hand, is not extracted during the surgery.
During the operation, the surgeon connects the blood vessels of the donated pancreas with the patient’s blood vessels. The organ is usually implanted with a donated portion of the duodenum, whereby this part is also fused directly with the recipient’s intestine or bladder.
In cases where the pancreas transplant is also associated with a kidney transplant, the procedure can take up to six hours.
When is a pancreas transplant performed?
The pancreas is the organ responsible for producing insulin, an anabolic hormone capable of lowering blood sugar levels. Diabetic patients are characterized by an imbalance in insulin production or its absence.
Pancreas transplantation allows the physiological ability to produce insulin to be recovered, reducing the alterations and complications associated with diabetes. However, this procedure is not considered the standard of treatment.
It is usually aimed at patients with type 1 diabetes mellitus, due to the need for external and continuous administration of the hormone. However, it has been shown that some patients with type 2 diabetes mellitus may also benefit from this intervention.
The association between diabetes and kidney disorders is what motivated the development of the surgical technique. This fact explains why most procedures are performed concurrently with or prior to a kidney transplant.
Risks associated with the intervention
Pancreas transplantation is an invasive surgical procedure, so it is not without complications, as is the case with other transplants. General risks of the surgery include adverse drug reactions and respiratory disorders associated with anesthesia.
On the other hand, there are typical complications of pancreas transplantation, among which the formation of blood clots, fistulas, inflammation of the pancreas, infections and organ rejection stand out.
1. Thrombosis
Thrombosis is one of the most common risks of pancreas transplantation ; it manifests itself in the first days after surgery. Thrombi usually form in the venous system as a result of vascular injury or hemodynamic changes.
This complication is responsible for the early loss of the donor organ in 5 – 6% of cases. To prevent this risk, after surgery, the specialist usually prescribes heparin and antiplatelet agents.
2. Fistulas
They are pathological communications that can occur on the junction line with the donor organ. In the early stage they are the result of technical errors or reduced blood flow in the tissue, while the late stage is associated with viral infections or organ rejection.
Currently their incidence has decreased thanks to the improvement of medical techniques. Fistulas typically require surgery and specific medical treatment.
3. Pancreatitis
Inflammation of the pancreas is an immediate postoperative complication. It is a consequence of the type of conservation before the intervention and manipulation of the organ. In most cases, pancreatitis is self-limiting and does not affect the functioning of the organ.
4. Infections
Immunosuppression and diabetes itself increase the risk of infections. Antibiotic therapy and continuous monitoring are therefore essential.
5. Acute rejection
Rejection of the donated pancreas is an event that occurs in 20% of transplant cases. In this situation, timely intervention is essential to obtain the best prognosis in the patient.
Preparation for pancreas transplant
The pancreas transplant requires physical and psychological preparation, since it will be conditioned by some variables before, during and after the operation.
Before the surgery
Once the need for pancreatic transplantation has been identified, the specialist provides the patient with information on the specialized facilities. The patient is free to choose the structure of preference.
The medical team will begin a comprehensive patient assessment period which usually lasts from one to two months. A series of analyzes will also be carried out to certify the recipient’s state of health. Among the exams we remember:
- Blood analysis.
- HIV test.
- Chest X-ray.
- Tests of kidney function.
- Electrocardiogram and echocardiogram.
- Psychological assessment.
Once eligibility is established, the facility places the patient on a waiting list, based on the patient’s health and needs. The waiting period for a pancreas transplant can range from a few months to a few years.
While waiting for the surgery, it is important to stay healthy. For this it is good to adhere to the following recommendations:
- Go to all medical examinations and follow the instructions of the specialist.
- Maintain a healthy weight with a balanced diet and mild to moderate exercise.
- Avoid the consumption of alcohol and tobacco.
- Carry out relaxing activities that promote psychological well-being.
- Prepare the necessary for the transfer to the hospital.
During the surgery
Pancreas transplantation is performed under general anesthesia which can be administered by inhalation or intravenously.
The surgery is performed through an incision in the abdomen, which will be used to implant the donor organ and make its correct connection with the other organs of the recipient.
The medical team will closely monitor all of the patient’s vital signs. The procedure usually lasts 3 hours but can be prolonged in the case of simultaneous transplantation.
After the surgery
Once the surgery is finished, the patient will remain in intensive care for a couple of days to monitor for any complications; he will then be transferred to the intensive care unit for a week.
Upon discharge, the medical team may ask the patient to stay close to the center for two or three months. Strict medical monitoring and surveillance is essential.
The specialist will prescribe several medications that must be taken to avoid complications. Immunosuppressive drugs help the body accept the new organ and prevent acute rejection. However, it is also important to take antibiotics to prevent infections from developing.

Dietary advice after pancreas transplantation
Once home, it is essential to follow a healthy diet that favors the recovery of the pancreas and the maintenance of its functionality. At the same time, diet combined with exercise allows for weight control.
Evaluation by a nutritionist will be essential. In general, the main tips for a healthy diet after pancreas transplantation are as follows:
- Diet rich in animal proteins such as fish, poultry and lean meat.
- High percentage of fruit and vegetables, at least 5 servings a day.
- Foods rich in fiber.
- Low-fat dairy products.
- Reduction in the consumption of salt and saturated fats.
- Reduction in caffeine and alcohol consumption.
- Drink lots of water and fluids.
- Avoid fruit and acidic juices like grapefruit and orange.
Medicines are your best allies after a pancreas transplant
With a successful pancreas transplant, the patient will no longer need to take insulin for the rest of their life. In addition, the incidence of diseases associated with high blood sugar levels will be reduced.
However, in most cases, the body constantly risks rejection of the new organ. Therefore, prolonged immunosuppressive therapy will be required, which could be maintained for the rest of life. In addition, constant medical supervision offers the tools for a healthy and uncomplicated life.